What do online users want from HIV/STI risk calculators?

Risk calculators for HIV and other sexually transmitted infections (STIs) use answers to a set of sociodemographic characteristics (e.g., age, sex, ethnicity, geographic location), health status, or behavioural questions to estimate a person’s risk for developing or acquiring HIV and STIs. They can also indicate the most appropriate action for users to take.
Identifying the features for online risk calculators to be appealing to STI clinic clients and testing service providers is a significant task given that more and more individuals turn to the Internet to find sexual health information and a lot of sexual health services and tools are offered online.
Speaking to potential end-users
For this reason, our team set out to figure out the content and format features that are desirable to potential end-users of these online tools. We invited clients and service providers from the STI Clinic at the British Columbia Centre for Disease Control to participate in focus groups. Clinic clients and service providers interacted with and discussed a few HIV/STI online risk calculators with different content and question characteristics, target audiences, completion lengths and recommendation messages.
Six desirable content and format features of HIV/STI risk calculators
From five discussion sessions with a total of 12 STI clinic clients and five service providers, we identified six main desirable features for this kind of online tools to be appealing to them:
- Provide personalized risk assessments: End-users want risk assessments that reflect their specific sexual behaviours and HIV/STI-related concerns.
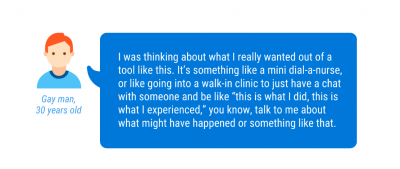
- Customize nuanced risk assessment and incorporate tailored educational information: End-users want sophisticated assessments that go beyond merely providing generic messages and recommendations.
- Supply numeric risk estimates: For some end-users, especially those with sophisticated sexual health knowledge, measurable or numeric estimates are an essential element in making sense of risk information.
- Use non-stigmatizing framing and inclusive design: The language employed in the tools must avoid equating sex with risk or judging users for being sexually active. The design has to be inclusive of different genders, sexual behaviours, racial and ethnic identifications and languages.
![Service provider, 13 years of STI prevention work. "They [risk calculators] do seem to be quite narrowly focused. They're always erring on the side of "everything is a risk." That whole kind of model of any time you have sex you're at risk for everything, and sex is a really diseasey kind of thing to be doing. So every time you touch another human being, "you're at risk for something." A lot of risk calculators work on that assumption. They bring that public health idea from the past with them."](http://blog.catie.ca/wp-content/uploads/Oralia_Quote-2-v2-400x267.png)
- Include explanations and actionable next steps: End-users must understand the questions asked and results provided. End-users must also receive information on concrete actions they could take next to address HIV/STI prevention and testing.
- Develop effective and appropriate branding: End-users want adaptable and reliable tool interfaces, recognized institutional backing of the tool and transparency about the privacy of the information provided in the calculation.
What are the implications?
For developers of online HIV/STI risk calculators, these insights highlight how critical it is to incorporate user-oriented feedback in the design of online sexual health tools. Failing to consider users’ desirable features in these tools’ designs can negatively impact their actual acceptability among end-users.
For researchers, these findings underscore the complexities of balancing and implementing characteristics that appeal to different end-users in an online environment. When well-designed and endorsed by reputable institutions, online tools can complement traditional sexual health services and help fulfil a public health prevention goal.
Find out more:
If you want to find out more about this project, check out our team’s recent publication discussing in more detail end-users’ preferred characteristics of HIV/STI risk calculators, or visit our research team’s website.
Oralia Gómez-Ramírez, PhD, is a postdoctoral research fellow with the Online Sexual Health Services program at the British Columbia Centre for Disease Control and the School of Population and Public Health at the University of British Columbia. She is a social scientist with expertise and experience in digital public health, implementation science, health equity, HIV/STBBI prevention, institutional and feminist ethnography, gendered labour and racialized class, and program evaluation. She is supported by a Canadian HIV Trials Network postdoctoral fellowship and a recipient of the Michael Smith Foundation for Health Research Trainee Award.
Hsiu-Ju Chang, MSc, has worked in multidisciplinary research projects that improve marginalized populations’ health and wellness over the last decade. She is currently the research manager of the Digital Sexual Health Initiative (DiSHI) housed within the Clinical Prevention Services unit at the British Columbia Centre for Disease Control.
