What does it take to build a successful digital STBBI testing service?
Access to testing for sexually transmitted and blood borne infections (STBBI) can be difficult for many people due to long travel distances, stigma, privacy concerns and lack of culturally safe services. Digital STBBI testing programs that let people request a lab form or self-collection kit online without seeing a healthcare provider are one way of overcoming these barriers.
However, there isn’t a lot of practical guidance available about how to develop complex digital health services like these. The Digital & Sexual Health Initiative team at the British Columbia Centre for Disease Control (BCCDC) and University of British Columbia has tried to fill this gap. We created a how-to guide based on our experience developing and implementing GetCheckedOnline, a digital STBBI testing program that has been running in B.C. for a decade.
About GetCheckedOnline
GetCheckedOnline lets people test for STBBIs by creating an account, getting a lab form, submitting specimens at a local lab and getting results online or by phone. Launched in 2014, GetCheckedOnline is now available in nine municipalities across the five health regions of B.C. with more than 3,000 test visits per month. Evidence has shown that GetCheckedOnline increases testing uptake and frequency, reaches people who are more likely to have an infection, empowers people to test, and improves health equity, among other impacts.
What makes digital STBBI testing work?
Running this program has been a dynamic experience that requires proactive planning, collaboration and adaptability to maximize benefits for both users and healthcare providers. Drawing on consultations with 45 staff from agencies and organizations involved with GetCheckedOnline from initial planning to its current state, we have identified four key components for building a successful digital STBBI testing service.
1. Understand and evaluate
We found it important to evaluate and gather information at all stages of implementation. This allows digital STBBI testing services to address real needs and focus on equity, sustainability and costs. If developing a similar service, we recommend:
- Identifying health equity gaps and priority populations: Define who the service intends to reach. For GetCheckedOnline, we wanted to address testing barriers for populations disproportionately impacted by STBBIs.
- Identifying teams, implementation partners and skill sets: Determine the critical skills and expertise the service needs (for example, clinical, IT, privacy, user-centred design, or project management skills), as well as whether these are already possessed internally or need to be outsourced.
- Building in evaluation and cost assessment mechanisms: Create a clear evaluation framework with measurable outcomes and clear budget metrics. GetCheckedOnline uses routinely collected program data to evaluate its effectiveness and conducts research for supplementary evidence.
2. Secure and maintain partnerships
In our experience, digital services depend on support from a diverse group of partners, including internal teams (like IT and clinical staff) and external organizations (like community groups and laboratories). We recommend:
- Building trust and creating a shared vision: Involve partners early and often to define shared goals and promote cross-disciplinary discussions. During the early planning for GetCheckedOnline, we established working groups with clinicians and community organizations to ensure goals were collectively defined and refined over time.
- Demonstrating the service’s value: Use research, metrics and case studies to highlight evidence-based benefits. GetCheckedOnline built support for subsequent scale-up by sharing pilot data on increased testing uptake and reduced barriers to care.
- Addressing concerns and barriers: Spot concerns early on, such as privacy, data security or workload challenges, and address them with clear, customized solutions. For GetCheckedOnline, closely engaging with IT and privacy experts ensured the platform was built to meet data security standards.
3. Develop a flexible and scalable intervention
Digital health services need to grow and adapt over time to respond to changing needs, policies and guidelines. We recommend:
- Focusing on community and clinical needs: Design the service with users in mind. We conducted focus groups, usability testing and beta testing with users to continuously improve the website designs.
- Building and improving incrementally: Start small using pilot projects or phased rollouts to test functionality and fix issues early. GetCheckedOnline first focused on clients of BCCDC’s clinics before expanding to Vancouver and then scaling up to different regions in B.C.
- Making sure systems work together: Connect the digital service with existing healthcare infrastructure, such as lab reporting and surveillance systems. GetCheckedOnline works with private labs already operating within the B.C. system, which facilitates specimen collection and data sharing.
- Designing for long-term success: Design the program to be as flexible and adaptive as possible. We work with a user experience (UX) designer to introduce new features over time.
4. Plan for long-term success
When developing and implementing GetCheckedOnline, we found that long-term planning was essential to make the service sustainable. While it is helpful to start small and go step by step, start the long-term planning early and continue planning throughout implementation. We recommend:
- Strengthening cross-sector collaborations: Maintain partnerships and build formal collaboration with existing partners through establishing agreements, for example.
- Having dedicated long-term staff and teams: Invest in diverse skills, including relationship building and project management. GetCheckedOnline benefits from a stable leadership and staff team with strong interpersonal skills.
- Creating a long-term strategy for funding: Advocate for including the service into existing healthcare budgets and explore multiple funding streams to help with sustainability.
- Integrating with existing systems and policies: Align the service with relevant health policies and strategies. For GetCheckedOnline, this included aligning testing with the clinical guidelines for STBBI testing in B.C.
Advancing health equity through digital STBBI testing
Digital testing services can address barriers to STBBI testing, expand access and improve health equity. For our program to achieve these outcomes, we paid careful attention to the four key components above, while always remaining flexible and persistent in the face of evolving challenges. When thoughtfully designed and continuously refined, digital STBBI testing services can transform the way people access care, making testing more accessible, inclusive and effective for all communities.
Getting hands on?
For program implementers, we also have an accompanying workbook to the how-to guide to help you develop your digital STBBI testing services.
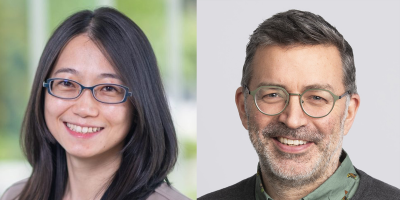
Hsiu-Ju Chang is a research manager at the BCCDC supporting the Digital & Sexual Health Initiative and other projects in the areas of sexually transmitted and blood-borne infections and tuberculosis.
Mark Gilbert is a public health physician of the BCCDC and an associate professor at the University of British Columbia School of Population & Public Health. Mark is the medical lead for the Online Sexual Health Services program at BCCDC and conducts research to support the development and implementation of internet-based approaches to sexual health service delivery such as GetCheckedOnline. Mark leads the research program Digital & Sexual Health Initiative, and holds an applied public health chair related to improving STBBI testing systems.
